In theory, dual eligibility — being eligible for both Medicare and Medicaid — sounds like a good setup. But historically, care in dual systems has been highly fragmented. There’s a lack of coordination which oftentimes leads to higher costs and lower quality of care.
To address these challenges, new changes to dual-eligible plans were rolled out this year. In our recent webinar, I explained everything you need to know about these changes so you can make sure your clients get the coverage they need and have confidence to navigate coverage rules and provider networks.
If we missed you at the webinar, watch the recording, or read through the key takeaways below.
How does dual eligibility work?
When a beneficiary is dually eligible (DE), it means they qualify for both Medicare and Medicaid. Medicare always pays first for Medicare-covered services, followed by any other health insurance they have, and then Medicaid kicks in. A dual-eligible beneficiary can choose between Original Medicare or Medicare Advantage.
Quick tip: Every state has its own way of designing and administering Medicaid programs. Make sure you check state sites to ensure you understand how all of the plans work in your specific location.
What are Medicare Savings Programs?
Medicare Savings Programs (MSPs) provide financial assistance to pay for Medicare Part A and Part B premiums. If qualified, MSPs might also pay Part A and Part B deductibles, coinsurance, and copayments. To qualify, beneficiaries need to have income and resources below a certain limit. If one of your beneficiaries qualifies for an MSP, they may also qualify for partial or full Medicaid coverage from their state.
There are four types of MSPs, all of which they should apply for through their state Medicaid office.
1. QMB (Qualified Medicare Beneficiary)
- The state helps pay for Part A and Part B premiums, deductibles, coinsurance, and copayments. Beneficiaries automatically get Extra Help. (QMB+ is an individual who qualifies for QMB and also meets the requirements for full Medicaid benefits).
2. SLMB (Specified Low-Income Medicare Beneficiary)
- The state helps pay for Part B premiums (but they have to have both A and B to qualify). Beneficiaries automatically get Extra Help. (SLMB+ is an individual who qualifies for SLMP and also meets the requirements for full Medicaid coverage).
3. QI (Qualifying Individual Program)
- The state helps pay for Part B (but they have to have both A and B to qualify). Beneficiaries apply every year to stay in this program. Beneficiaries automatically get Extra Help.
4. QDWI (Qualified Disabled & Working Individual Program)
- The state helps pay for Part A premiums only. Beneficiaries have to apply for Extra Help.
Quick tip: If their limits are higher than what’s listed, they may still qualify for other state programs. Encourage your clients to check with their state Medicaid agency.
What is a D-SNP?
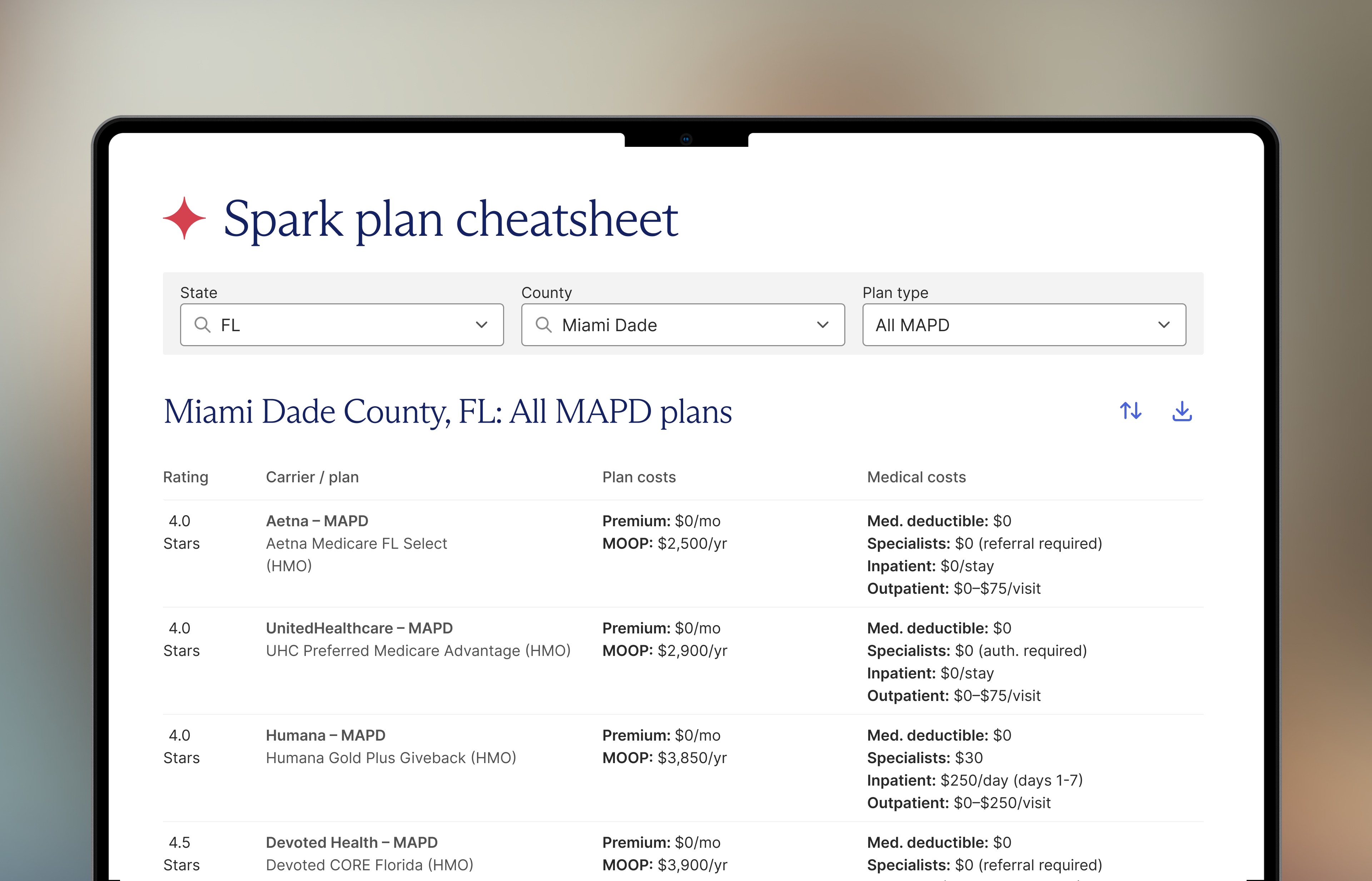
Dual Eligible Special Needs Plans, better known as D-SNPs, are Medicare Advantage plans designed for dual-eligible beneficiaries. They provide Medicare-covered services, and in most cases, supplemental benefits. You’ll need to check with carriers and state guidelines to determine what Medicare Savings Programs qualify for a D-SNP.
The type of D-SNP your beneficiary is on will impact the degree of coordination and coverage of Medicaid benefits. Here are the different types:
1. HIDE (Highly Integrated Dual Special Needs Plan)
- Improves coordination of care. Must cover behavioral health or long-term services and supports. May exclude some Medicaid services.
2. FIDE (Fully Integrated Special Needs Plan)
- Fully integrates coordination of care. Provides nearly all Medicaid services including long-term services and supports, behavioral health, home health, and durable medical equipment. Requires Exclusively Aligned Enrollment (EAE). May be eligible for payment adjustments.
3. AIP (Applicable Integrated Plans)
- Subtypes of HIDEs and FIDEs.
4. CO (Coordination-only Dual Eligible Special Needs Plan)
- Provides Medicare covered services. Coordinates the delivery of services, but is not as integrated as the three plans above.
What are the enrollment periods for D-SNPs?
As of 2025, there are two enrollment periods for D-SNP beneficiaries:
1. SEP (Special Enrollment Period)
- A three-month period, used if the dual-eligible beneficiary gains, loses, or has a change in Medicaid status.
- Plans: MAPD or PDP
2. SEP-INT (Integrated Special Enrollment Period)
- An enrollment period that is available monthly for integrated plans.
- Plans: D-SNP FIDE, HIDE, and AIP.
Quick tip: Always check carrier websites for eligibility before doing an enrollment. Sunfire will be adding a lookup feature in the near future.
How can I approach these conversations?
As an agent, you understand the power of getting out into your community and connecting with potential beneficiaries. Continue going to food banks, senior centers, and bingo halls to chat with folks. Another great approach is to offer education sessions to teach people about dual eligibility and enrollment periods. Position yourself as the expert on this topic. In most cases, the more you educate, the more referrals you get.
When you’re speaking 1:1 with people, ask them questions to learn about their needs. Try something like: How much are you making a month on your social security income? If it’s below your state’s income threshold, you know it’s a good opportunity to educate them on the available programs. Get them the phone numbers they need and the address for the Medicaid office — make it easy for them.
Quick tip: If you already have clients on D-SNP plans, reach out to them and educate them on the SEP-INT changes. Stay in touch with them throughout the year whether that’s by phone, email, or text to see if they need assistance navigating benefits on their plan. Spark’s Retention Program has some good resources for this.
Taking your next steps
If you’re an agent with Spark looking for more resources on dual eligibility, check out the training and compliance pages on the Spark Help Center. We also have resources on how to build a winning D-SNP strategy and what you need to know about Extra Help/LIS.
For Spark and non-Spark agents, bookmark these for future reference:
- Medicare.gov
- Your state Medicaid website
- LIS Guide from SSA
- Carrier portals
- Sunfire (lookup tool coming soon!)
- Benefits CheckUp site
Follow Spark on LinkedIn, Facebook, and Instagram for more industry advice and success stories from top agents and principals







.png)



.png)

.png)





.png)

.png)




.png)






.png)
.png)




.png)

.jpeg)

.png)





.png)


.jpeg)







.png)

.png)

.png)
.png)






