As an agent, your job isn’t just to enroll beneficiaries, but to help them thrive. That starts with making sure they know about programs like Extra Help, which could save them hundreds on prescriptions every year.
In our recent webinar, we broke down one of the most powerful tools for lowering medication costs for low-income clients: Low Income Subsidy (LIS), also known as Extra Help. This federal program eases the financial burden of Medicare Part D — but many eligible clients still don’t know about it.
Didn’t catch the webinar? We’ve got you.
Check out the key takeaways below, or watch the full recording here.
What is Extra Help?
Think of Extra Help as a safety net for prescription drug costs under Medicare Part D. It helps cover:
- Monthly premiums
- Annual deductibles
- Prescription copays
Extra Help is estimated for 2025 to be worth about $6,200 a year to the beneficiaries who qualify.
Who qualifies — and how?
Eligibility is based on income and resources, and thresholds change each year. For 2025, the resource limit for a single individual is $17,635. For a married couple living together, the threshold is $35,160. Most beneficiaries qualify either by meeting the income and asset limits, or being dually eligible for both Medicare and Medicaid.
Anyone on full Medicaid, a Medicare Savings Program (MSP), or Supplemental Security Income (SSI) usually gets Extra Help automatically, but it’s worth verifying enrollment to avoid lapses.
Here’s the kicker: many clients who qualify never apply — either because they simply don’t know about it or assume they won’t be eligible.
That’s where you come in. As an agent, asking a few screening questions and assisting clients with the application process can make a huge difference.
Actionable steps for agents
Here’s what you can do right now to support your clients:
- Screen for eligibility: Ask about income, assets, and Medicaid/SSI enrollment. Even if clients don’t qualify for full Extra Help, they might qualify for other assistance programs.
- Use the SSA application: Offer to walk clients through the Social Security Extra Help application in person, over the phone, or send them the link.
- Check plan alignment: Make sure your client’s drug plan matches their needs, especially once Extra Help kicks in. Clients with Extra Help can change their Prescription Drug Plan (PDP) monthly.
- Educate and advocate: Build awareness about this program by including Extra Help in your Medicare 101 sessions and bring it up during AEP and SEP conversations. Listen to your clients to catch any signs that they might need extra assistance — for example, if they express having trouble paying for groceries or utilities.
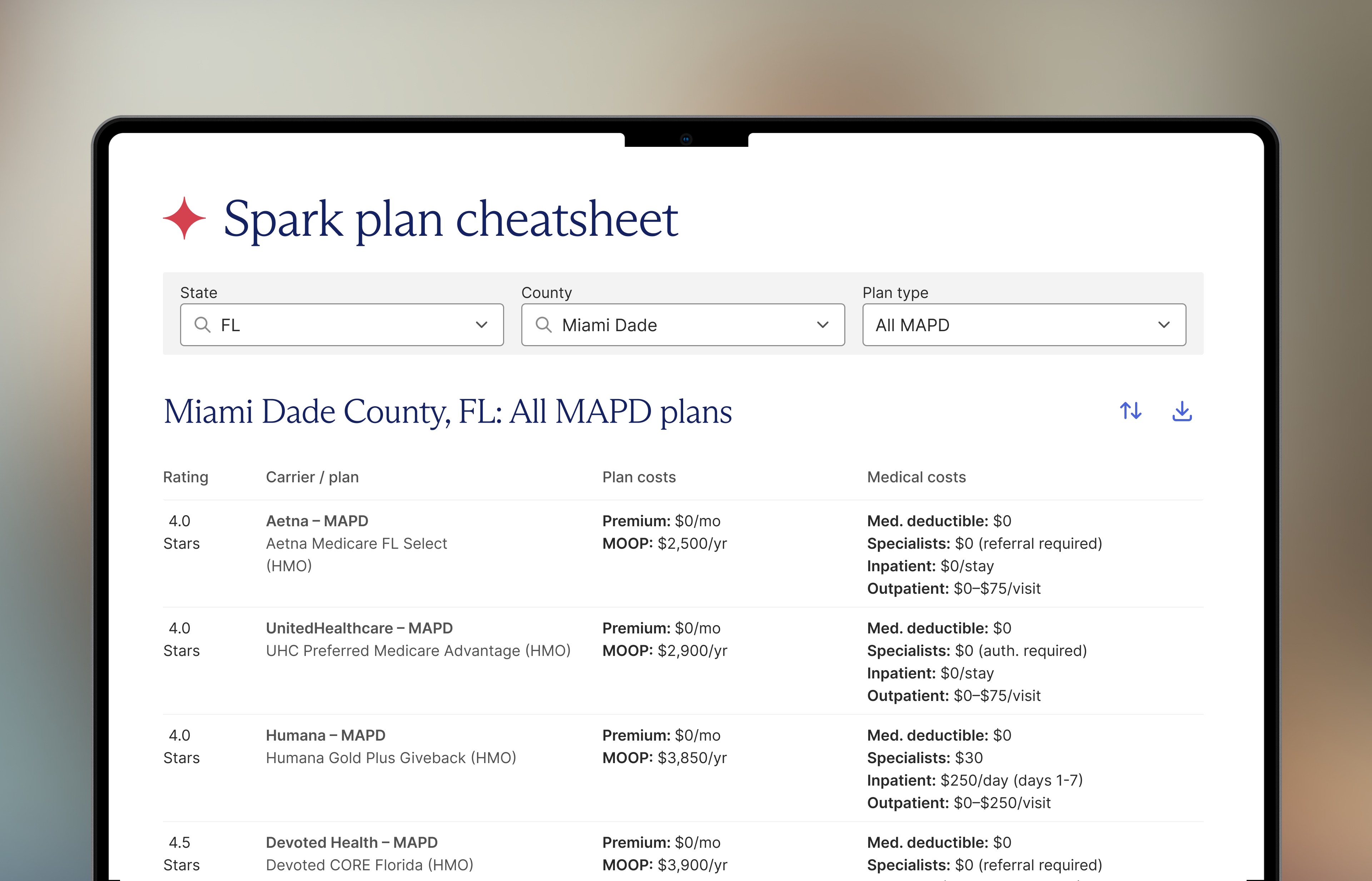
- Use Spark tools: Spark provides bilingual materials, application support, and year-round outreach campaigns to help you connect with LIS-eligible clients.
Helping clients save money is a key part of an agent’s job. Whether beneficiaries are low-income, dual eligible, or just overwhelmed with prescription costs, Extra Help could be a game-changer — and you can be the one who opens that door.
This kind of education benefits your business as well. When you spend time educating people on valuable benefits, you build their trust—which in time could lead to new referrals.
Want support reaching LIS-eligible communities?
Reach out to local businesses and events where you can make contact with potential clients.
Spark agents can also take advantage of our materials, tools, and templates. Learn more about the platform agents can’t live without: Book a demo.
FAQs
- How can I assist clients in applying for Extra Help?
Clients can apply online through the Social Security Administration’s website, over the phone by calling 1-800-772-1213, or by visiting their local Social Security office. As an agent, you can guide them through the application process, help gather necessary documents, and ensure they understand the benefits. - What should I do if a client was denied Extra Help previously?
Encourage them to reapply, especially if their financial situation has changed. Income and resource limits are adjusted annually, and changes in circumstances may make your client newly eligible.
- Can clients switch their Medicare drug plans after receiving Extra Help?
Yes. Beneficiaries who qualify for Extra Help can switch their Prescription Drug Plan (PDP) monthly.
- Can a client automatically be eligible for Extra Help?
Beneficiaries qualify for Extra Help automatically if:- They get full Medicaid coverage
- They get help paying their Part B premiums from a Medicare Savings Program
- They receive SSI benefits
Follow us on Linkedin, Facebook, and Instagram to learn about upcoming webinars and training sessions.











.png)




.png)




.png)





.jpeg)


.png)
.png)

.png)

.png)

.png)
.png)
.png)



.png)











.png)




.png)



.png)

.jpeg)
.png)